Hannah Bridges
Mum of two, Midwife and Pregnancy/postnatal Yoga Teacher
@wellbeingmidwife
Summary
Pelvic Girdle Pain (PGP) affects a significant number of pregnancies, with 1 in 5 expectant mothers experiencing its symptoms 1. Despite its prevalence, PGP is not a normal part of pregnancy and should not be dismissed as such. This blog post sheds light on PGP, its symptoms encompassing pelvic discomfort and stiffness, and emphasizes the importance of seeking early diagnosis and appropriate management. It aims to provide insights into the challenges faced by those dealing with PGP, featuring a personal account from Hannah, who shares her experience with severe PGP during her second pregnancy. The post also offers practical advice on managing PGP, including seeking support from healthcare professionals, staying active within pain limits, and utilizing various coping strategies. For a comprehensive understanding and support network, the post directs readers to resources like @thepelvicpartnership and encourages open communication with friends, family, and healthcare providers.
What is it?
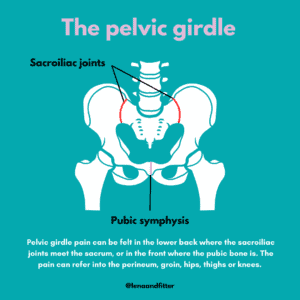
Pelvic girdle pain (PGP) affects 1:5 pregnancies, so it is relatively common but not normal. In most cases, it is treatable and not something women should just ‘put up with.’ PGP is the umbrella term for all pelvic pain and stiffness, including the symphysis pubis (pubic joint), hips/thighs, and sacroiliac joints in the lower back. Symptoms include difficulty walking, mobility issues, pain when standing on one leg or opening your legs, and clicking and grinding in the pelvic area. It can happen at any point during pregnancy or postnatally.
What helps?
Getting a diagnosis as early as possible will help manage your symptoms. This is usually done by a physiotherapist whom your midwife can refer you to. Aim to keep active but within pain limits and avoid anything that makes your pain worse. Accept any help with daily tasks and childcare. Even climbing the stairs, pushing a shopping trolley, and getting in and out of the car can be difficult.
Hannah’s Experience
I had severe PGP in my second pregnancy and was shocked by how debilitating the condition was. My mobility was limited to the point I could barely walk some days – even going up and down the stairs was a mammoth task. My mental health suffered as a result, particularly around feelings of guilt that I couldn’t get on the floor to play with my three-year-old or even walk her to nursery. Emotional support is really important as PGP can be so tough and restrictive. Be kind to yourself. I found Manual therapy from a specialist physiotherapist and chiropractor helpful. A support belt, TENS machine, gentle exercises like swimming/yoga, baths, hot/cold therapy, strengthening exercises, pregnancy massage, and pain relief. *Please seek advice before trying any of these to ensure they suit your pregnancy.
Where can I seek support/advice?
Your midwife and physiotherapist should be able to support you with getting a diagnosis. @thepelvicpartnership is a great source of support and advice. Ensure your friends, family, and work know that you have PGP and understand how it affects you and how they can help you. Speak to your GP if you are struggling emotionally, feel you need time off work or prescribed pain relief.
You can find more from Hannah on her Instagram and Facebook @wellbeingmidwife or by dropping her an email at we**************@*****ok.com
Links to other resources
 Websites
Websites
NHS | Pelvic Pain in Pregnancy
References
- Royal College of Obstetricians and Gynaecologists (2015) ‘Pelvic Girdle Pain and Pregnancy’